Members Rate Their Provider Experience
Date: 03/24/25
Each year, Superior HealthPlan conducts five Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys for Superior Medicaid (STAR, STAR Health, STAR Kids, STAR+PLUS), CHIP, STAR+PLUS Medicare Medicaid Plan (MMP), Wellcare By Allwell (HMO and HMO DSNP) and Ambetter from Superior HealthPlan members.
The CAHPS surveys asks members/patients to rate their overall health-care experience, including interactions at their provider’s office. When members evaluate this experience, they often combine their provider interactions with their health plan encounters as well. Superior believes it is beneficial to collaborate with our provider community to enhance the member’s journey in receiving care and services.
What were Superior’s 2024 CAHPS Survey Results?
Survey results are trended over time to evaluate against Superior goals and improvements, analyze results with available data, including complaint, denials and appeals, and feedback from Superior member and provider advisory groups. Typically, these results impact National Committee for Quality Assurance (NCQA) health-plan rankings, Medicare Star ratings, Qualified Health Plan (QHP) ratings, and Superior member experience initiatives.
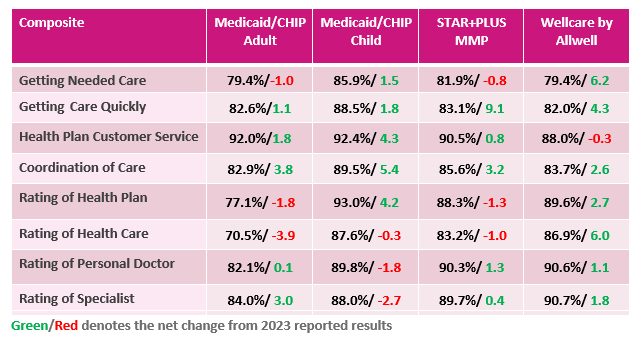
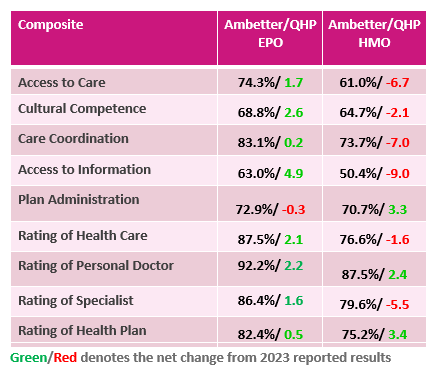
In 2024, CAHPS surveys were completed by Medicaid, CHIP, Ambetter, Wellcare By Allwell and MMP members. Please review the 2024 survey results below:
Survey Results for Medicaid/CHIP, MMP and Wellcare By Allwell Members
Survey Results for Ambetter Members
The CAHPS survey is administered annually by an external survey vendor, SPH Analytics, using the survey protocol defined in current Healthcare Effectiveness Data and Information Set (HEDIS) Specifications. For more information about how providers can impact the member care experience, please download the CAHPS Provider Tip Sheet, found under Quality Resources on Superior’s QI Program webpage.
For any questions, please call Provider Services at 1-877-391-5921
